

Ovalbumin (OVA) was used to induce asthma
1. Background
Asthma is a chronic airway inflammatory disease characterized by variable airflow obstruction, airway hyperresponsiveness (AHR), and airway inflammation. The main clinical symptoms of asthma are shortness of breath, wheezing, cough, and increased mucus production after exposure to allergens. Its pathogenesis is caused by a complex interplay between genetic, epigenetic, and environmental factors.
Different pathological changes are mediated by a variety of cells involved in the immune response, such as airway epithelial cells, eosinophils and T lymphocyte subsets. Among them, Th2 cells are considered to be dominant in hypereosinophilic asthma, accompanied by increased levels of cytokines IL-4, IL-5 and IL-13.
In recent years, the incidence of asthma has been on the rise worldwide, and due to the different causes and degrees of the disease, it has seriously affected the health and quality of life of patients. Therefore, the pathological study of asthma is particularly important.
The classic asthma model is an ovalbumin (OVA) -induced airway inflammation model. The model of acute asthma was established by multiple intraperitoneal injections of OVA for sensitization and aerosol inhalation of OVA for challenge.
2. Experimental Materials and Methods
Experimental material:
SD rats (Male, 6-8 weeks)
Ultrasonic atomizer (Manufacturer: Fulin Product No. : W001)
Ovalbumin (Manufacturer: Maclean's Product No. E6377)
Aluminum hydroxide (Manufacturer: Shanghai Test Sinopharm code: 20001060)
Modeling method: Adaptively feeding for 7 days, on the first and eighth days, normal saline containing 10mg ovalbumin and 200mg aluminum hydroxide was intraperitoneally injected. From the 15th day, Inhalation and provocation were started with aerosolized saline containing 1% ovalbumin, 30 min each time, once a day for 14 days, the lung tissue was collected at the end of atomization.
Evaluation indicators: Serum inflammatory factors and IgE detection, HE staining.
3.Validation
HE staining
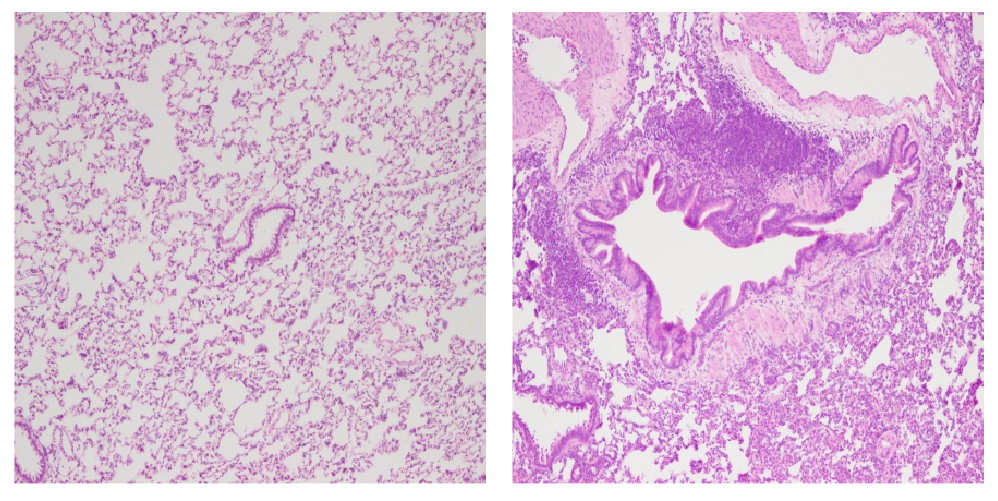
Normal group Model group
HE staining showed that the alveolar structure of lung tissue in the normal group was normal, and the bronchial epithelial structure was basically complete without obvious shedding. In the model group, the alveolar wall of lung tissue was significantly thickened, the alveolar cavity was reduced, the interval was widened, and the structure was disordered. A large number of inflammatory cells infiltrated the bronchi, blood vessels, and lung interstitium. The bronchial smooth muscle and basement membrane were significantly thickened, airway goblet cells proliferated, airway mucosa was irregularly proliferated, and some bronchial epithelial cells were exfoliated.
Serum inflammatory factors and IgE were detected
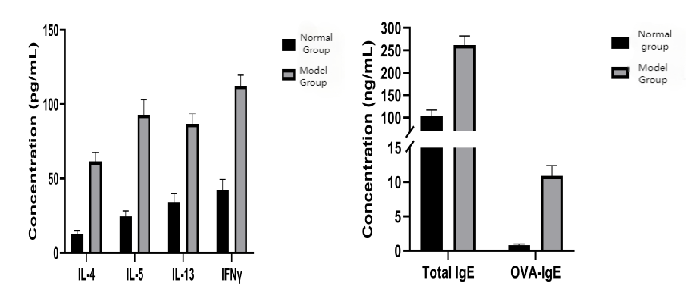
Results of serum inflammatory factors: The levels of serum IgE and IL4,IL5,IL13, IFNγ in the model group were significantly higher than those in the normal group.


